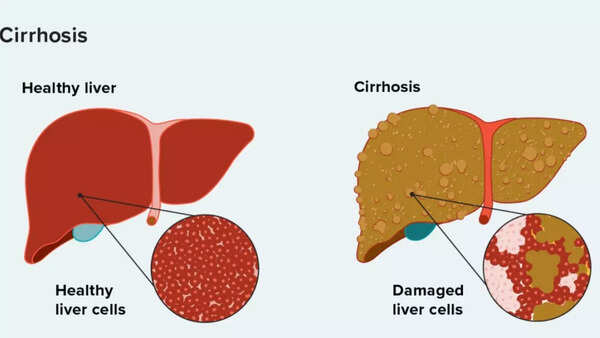
Cirrhosis of the liver is a chronic and progressive disease in which healthy liver cells are slowly replaced by scar tissue, impairing vital liver functions such as detoxification and nutrient processing. Common causes include chronic alcohol consumption, hepatitis B and C and non -alcoholic liver disease. Often, in the early stages, cirrhosis can lead to severe complications such as liver failure, if not treated. This detailed guidance studies its causes, symptoms, stages and available diagnostic and treatment options, emphasizing the importance of early detection and lifestyle change in the state management and preventing irreversible damage.
What is cirrhosis
Cirrhosis occurs when chronic liver damage leads to persistent inflammation and scars (fibrosis). As the liver tries to cure itself, it forms a scar tissue instead of healthy cells. Over time, this tissue enhances the liver, breaking the necessary features such as:
- Filtering toxins from the blood
- Processing of nutrients, hormones and medicines
- Making bile for digestion
- Create proteins for thickening and immune defense
As the scars increase the liver loses the ability to recover, resulting in liver or liver disease.
Source: Cleveland Clinic
Cirrhosis of the liver : Early and advanced symptoms
Symptoms vary depending on the stage and the cause of the disease. Early warning signs can be vague, but they deteriorate as the condition.Early symptoms:
- Fatigue and weakness
- Loss of appetite or nausea
- Discomfort in the upper right abdomen
- Redness of palms (palm erythema)
- Spider anogy (on the skin, visible small blood vessels)
Extended symptoms
- Jaundice (yellowing of skin and eyes)
- Dark urine, pale stools
- Itching skin
- Swollen legs or abdomen (swelling and ascites)
- Confusion or memory loss (liver encephalopathy)
- Bruises and bleeding is easy
- Hormonal changes such as enlarged men’s breasts or missed periods

Liver cirrhosis: General causes
As depending on Clinic ClevelandCirrhosis-final result of long inflammation of the liver. Some of the most common reasons include:
- Alcohol associated with alcohol, liver disease
Chronic alcohol and liver scars. Repeated effects over time leads to alcohol hepatitis and eventually cirrhosis.
- Non -alcoholic fatty liver disease (nafld)
Associated with obesity, high cholesterol and diabetes, Nafld causes the accumulation of fat in the liver cells, causing inflammation.
- Chronic hepatitis B and C.
Both viral infections attack liver cells, leading to long -term damage and fibrosis. In particular, hepatitis C is often asymptomatic over the years.
- Autoimmune and genetic conditions
Autoimmune hepatitis, Wilson’s disease and hemoromatosis can also lead to cirrhosis, causing constant inflammation of the liver.
Stages of cirrhosis
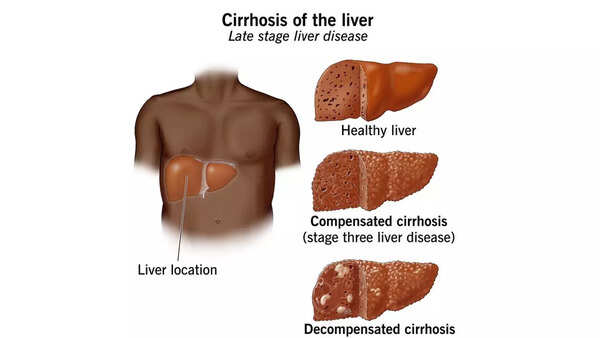
Source: Healthline
Cirrhosis develops at two main stages, depending on how much damage the liver has done.At this early stage, the liver is damaged, but still performs its basic functions. Many patients do not experience obvious symptoms, and cirrhosis may go unnoticed unless it is detected by blood tests and visualization.As the scars deteriorate, the liver can no longer function properly. The decompensated cirrhosis is marked by serious symptoms such as jaundice, fluid retention, bleeding and mental confusion. This stage is often life -threatening and may require liver transplants.
As diagnosed with cirrhosis
According to reports, early diagnosis is crucial for the control and slowing of the disease. Doctors can use:
- Blood tests for measuring liver enzymes, bilirubin levels and protein
- Visualization tests such as ultrasound, CT or MRI to detect liver changes
- Elastography to assess liver stiffness (scars)
- Liver biopsy for final diagnosis and reasons for identification
Is it possible to cure cirrhosis
The cirrhosis is not reverse, but with proper care, its progression can be slowed down and even stopped. Treatment focuses on managing the cause, improvement of quality of life and prevent complications.As cirrhosis, this can lead to severe and even mortal complications:
- Portal Hypertension (Increased Pressure in the Liver)
- Ascites (abdominal accumulation)
- Varical bleeding (internal bleeding from enlarged veins)
- Liver cancer (hepatocellular carcinoma)
- Failure in the kidneys and lungs
- Mental confusion or coma (liver encephalopathy)
A liver cirrhosis diet: what is there what to avoid
- Prioritize high protein meals
Include low -fat meat, fish, eggs, legumes, nuts and dairy products that help maintain muscle mass and avoid malnutrition.
- Include both vegetable and animal proteins
The combination supports balanced nutrition and promotes better liver function.Alcohol can accelerate liver scars and worsen the condition.
- Limit the processed products and trances
They can increase liver inflammation and further damage.Too much salt can cause fluid content and swelling (ascites).
- Avoid raw or ridiculous meat and seafood
Cirrhosis weakens the immune system, increasing the risk of food transmitted.
Manage cirrhosis through nutrition and medical support
While cirrhosis cannot be canceled, a diet that supports the liver can slow the progression of the disease, relieve symptoms and improve quality of life. Getting enough calories, proteins and nutrients, such as zinc, vitamin D and B vitamins is key. However, changes in diet may feel restrictive, especially if you avoid your favorite foods such as fast food or alcohol. Supporting a doctor or nutritionist is important for personalization of your plan and meet your nutritional needs. In some cases, supplements or medicines may also be recommended within your overall treatment.
Liver cirrhosis: Prevention tips
Cirrhosis usually does not develop overnight – this is the result of chronic liver damage over the years. Although some reasons such as genetic disorders cannot be avoided, many forms of cirrhosis can be prevented through a reasonable lifestyle and health. Early intervention and active health monitoring can significantly reduce the risk.
- Avoid alcohol and forbidden drugs
Alcohol is one of the leading causes of cirrhosis, especially when used to a large extent and regularly over time. The liver is responsible for the treatment of alcohol, and the excessive use of passionate and damage to liver cells, which leads to scars.
- Support a healthy weight
Being overweight increases the risk of non -alcoholic liver fat (NAFLD), a general condition that can go to cirrhosis if you do not treat. Obese liver disease is now one of the fastest causes of liver failure worldwide.What you can do: eat rich nutrients, balanced nutrition and stay physically active. Loss even 5-10% body weight can significantly reduce liver fat and inflammation.
- Vaccinated against hepatitis B
Hepatitis B-is a viral infection that can become chronic and cause long-term inflammation and liver damage. This is the main cause of cirrhosis worldwide.
- Diabetes management, cholesterol and blood pressure
Metabolic conditions such as type 2 diabetes, high cholesterol and hypertension associated with liver fat and cirrhosis.What you can do: regularly control blood sugar and cholesterol. Follow the doctor’s doctor’s advice, exercise and medicines to support these risk factors.
- Get regular liver reviews if you are at risk
Many people with liver damage in the early stages do not experience symptoms. That is why ordinary shows can be rescue, especially for people who have:
- Heavy -consuming alcohol
- Chronic Hepatitis B or C
- Obesity or diabetes
- A family history of liver disease
What you can do: Ask your healthcare provider for periodic liver function or visualization scan if you are in a high risk category.

Life with cirrhosis: Daily tips for better management
If you are diagnosed with cirrhosis, there is still a lot that you can do to slow down its progress and maintain the quality of life. Medical supervision combined with a healthy lifestyle can help you manage the symptoms and avoid complications.
- Keep track of the diet for the liver
- Your liver plays a central role in digestion and metabolism, so supporting its proper nutrition is important.
- Eat a lot of fruits, vegetables, low -fat proteins and whole grains
- Limit salt intake to reduce fluid accumulation (ascites)
- Avoid raw or undervalued mollusc
- Avoid alcohol and harmful medicines
Even a small amount of alcohol can accelerate liver damage after cirrhosis. Some drugs without a prescription, especially acetaminophen (paracetamol) and NSAIDs (such as ibuprofen), can also strain the liver. Always talk to your doctor before taking new medicines, supplements or herbal remedies.
- Regularly take the assigned medicine
The drug may be intended for the treatment of the main cause of liver damage (eg, hepatitis antivirus, diuretics for fluid content or lactulose with encephalopathy liver).The commission is key – do not miss doses and tell your doctor about any side effects.
- Monitoring by prevention signs
Cirrhosis can cause sudden complications, so it is important to remain vigilant. If you notice a doctor, contact your doctor:
- The swelling of the abdomen
- Confusion, drowsiness or change of personality
- Bleeding, bruising or dark fried stools
- A sudden weight gain or loss
- Stay in touch with your group
Regular observations with a hepatologist or gastroenterologist are vital. Your doctor will monitor the liver function, check the presence of complications such as varicose veins or liver cancer, and as needed to adjust treatment. You may need regular blood tests, ultrasound or endoscopy.*Refusal: This article is designed only for general information and educational purposes. This is not a replacement for professional medical advice, diagnosis or treatment. Always consult with a qualified healthcare provider with any questions that may arise against liver cirrhosis or any other medical condition.Also Read Is back pain the next global health crisis? That’s what it causes and 4 exercises you have to start now









